“Patellofemoral Pain Syndrome Explained: Signs, Symptoms, Risk Factors, Diagnosis, and Cutting-Edge Physical Therapy Approaches”
What is Patellofemoral Pain Syndrome (PFPS)?
PFPS is defined as pain occurring around or behind the patella that is aggravated by at least one activity that loads the patella during weight-bearing on a flexed knee, activities include running, climbing stairs, jumping, and squatting. PFPS is also called runner’s knee and anterior knee pain syndrome.1
PFPS is common in young adolescents, with a prevalence of 7–28%, and incidence of 9.2%. Studies in past have evaluated incidence in other populations, which shows female have more incidence of PFPS which is 6.5% whereas male is having 3.8%, with a prevalence of 12% in male and 15% in female.1
Risk Factors:2,3
- Muscular imbalance like quadriceps weakness or altered firing pattern or weakness of hip muscles.
- Overuse or wrong training patterns.
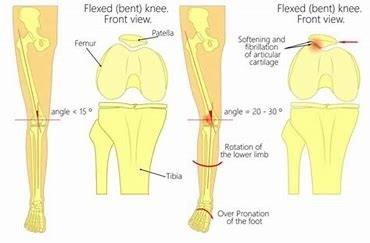
- Malalignment or altered biomechanics of hip, knee or foot.
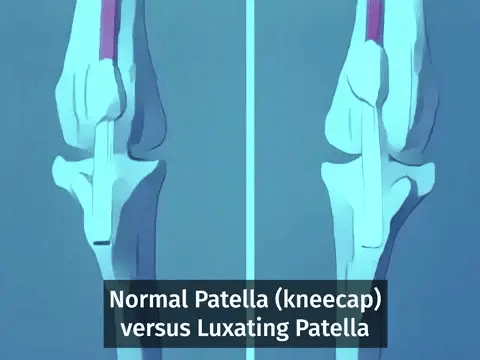
- Patellar hypermobility or anomalies like patella alta or hypoplasia of medial patellar facet.
- Tightness in iliotibial band or lateral retinaculum, quadriceps, hamstrings or glutues.
- Trauma or previous surgeries.
Diagnosis and examination:2,3
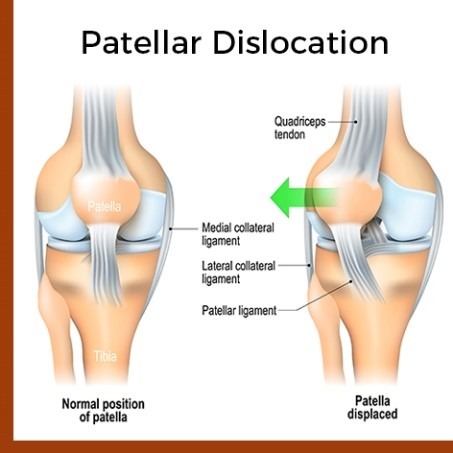
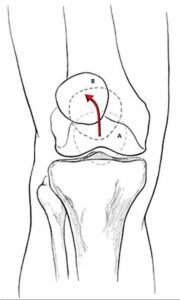
- Lateral patellar tracking sign: Suggests patellar maltracking as a result of tight lateral restraints or VMO dysfunction. ( J sign)
- Tenderness present in Medial or lateral retinaculum common in PFPS.
- Poping or clicking may present Patella may produce a palpable pop, click, or clunk with palpation during passive or active range of motion; may be a sign of patellar maltracking, perhaps caused by synovial hypertrophy, plica synovialis, or cyst formation; a popping sensation with marked lateral deviation of the patella in extension indicates patellar instability.
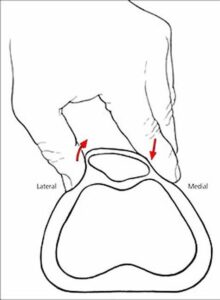
- Patellar glide: Assesses patellar mobility; displacement of less than one quadrant indicates tight lateral structures; displacement of more than three quadrants suggests patellar hypermobility caused by poor medial restraints.
- Patellar tilt test: lateral aspect of patella is fixed and cannot be raised to at least horizontal position indicates tight lateral structures.
- Patellar apprehension: pain or discomfort with lateral translation of the patella indicates lateral patellar instability as a cause of pain.
- Flexibility of quadriceps, hamstrings, ITB, hip flexors, and gastrocnemius can be assessed as compromised.
- Gait and foot analysis for pronated foot or compensatory gait mechanics.
Treatment:
1. Exercise Therapy:4,5,6,7
Strengthening exercises: Isometric exercises while the knee is fully extended used at the beginning of the therapy, because it minimizes stress on the patellofemoral-joint. Straight-leg exercise, patient elevates extended leg and holds it for 10secs or pillow squeeze exercise Patient sits comfortable with his trunk supported. Both knees extended. Placing a pillow/towel under one knee Patient is asked to push the pillow/towel in the table by extending his or her knee. Later on which are progressed to closed and open chain exercises like Squats in pain free range or terminal knee extension. Strengthening of VMO and hip muscles are also added to off load the knee joint in activities.
Stretching of targeted muscles: Tightened iliotibial tract, hamstrings, gluteus and quadriceps stretching is given passively to give better results with long duration of hold to improve muscle flexibility.
Core Stabilization exercises: It enhances the overall stability and reduces knee stress, proper engaging of all core muscles is taught in rest as well as during exercises or activities.
2. Proprioceptive Training:8,9
Exercises are designed to improve proprioception and balance, which helps in correcting movement patterns and reducing knee pain as proprioception of both the knees is altered. It reduces the risk of falls or further injuries in future.
3. Biomechanical Assessment and Correction: 1,2,3
Proper gait evaluation helps in correction of abnormal gait adapted because of pain or because of altered mechanism of foot, in such cases footwear adjustments or customized orthotics along with exercises helps better.
4. Manual therapy:
Techniques such as joint mobilizations, soft tissues release of tightened structures, and Myofasical release can be used to address muscle imbalances.
5. Kinesiotaping: 1,3
Specific techniques are used in tapping to support and prevent lateral shifting of patella, helps in pain reduction and mal tracking of patella.
Patellofemoral Pain Syndrome is a manageable condition with appropriate intervention. Early diagnosis and a tailored physical therapy program are key to alleviating symptoms and improving knee function. If you suspect you have PFPS, consult us we will help you develop a personalised treatment plan. With the right approach, you can effectively manage PFPS and return to your daily activities with greater comfort and ease.
References:
1. Crossley KM, Stefanik JJ, Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50(14):839-843. doi:10.1136/bjsports-2016-096384
2. Dixit S, DiFiori JP, Burton M, Mines B. Management of patellofemoral pain syndrome. Am Fam Physician. 2007;75(2):194-202.
3. Bolgla, L., & Malone, T. (2005). Exercise prescription and patellofemoral pain: evidence for rehabilitation. Journal of Sport Rehabilitation, 14(1), 72-88.
4. Tang, S. F., Chen, C. K., Hsu, R., Chou, S. W., Hong, W. H., & Lew, H. L. (2001). Vastus medialis obliquus and vastus lateralis activity in open and closed kinetic chain exercises in patients with patellofemoral pain syndrome: an electromyographic study. Archives of physical medicine and rehabilitation, 82(10), 1441-1445.
5. Irish, S. E., Millward, A. J., Wride, J., Haas, B. M., & Shum, G. L. (2010). The effect of closed-kinetic chain exercises and open-kinetic chain exercise on the muscle activity of vastus medialis oblique and vastus lateralis. The Journal of Strength & Conditioning Research, 24(5), 1256-1262.
6. Tang, S. F., Chen, C. K., Hsu, R., Chou, S. W., Hong, W. H., & Lew, H. L. (2001). Vastus medialis obliquus and vastus lateralis activity in open and closed kinetic chain exercises in patients with patellofemoral pain syndrome: an electromyographic study. Archives of physical medicine and rehabilitation, 82(10), 1441-1445.
7. Benjafield, A. J., Killingback, A., Robertson, C. J., & Adds, P. J. (2015). An investigation into the architecture of the vastus medialis oblique muscle in athletic and sedentary individuals: an in vivo ultrasound study. Clinical Anatomy, 28(2), 262-268.
8. Nakagawa, T. H., Muniz, T. B., Baldon, R. D. M., Dias Maciel, C., de Menezes Reiff, R. B., & Serrão, F. V. (2008). The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clinical rehabilitation, 22(12), 1051-1060.
9. Akseki, D., Akkaya, G., Erduran, M., & Pinar, H. (2008). Proprioception of the knee joint in patellofemoral pain syndrome. Acta orthopaedica et traumatologica turcica, 42(5), 316-321.
“Advance Therapy blogs and clinical information are educational resources by Advance Therapy clinical employees. The content provided here represents the opinion of the individual author based on their expertise and experience. The content provided in this blog is for informational purposes only, does not constitute medical advice, and should not be relied on for making personal health decisions.”

